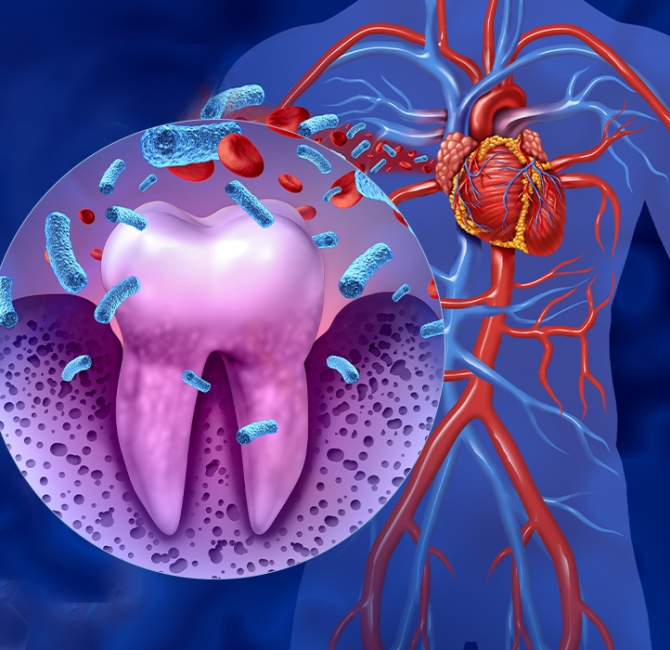
Inflammation is the body’s protective response to infection and/or trauma. Systemic inflammation is implicated in the onset and progression of several chronic diseases. Periodontitis is amongst the most common inflammatory diseases of the adult population and is a potential trigger of systemic inflammation.
The purpose of this review was to produce the most up-to-date systematic critical appraisal of all evidence regarding the effects of the treatment of periodontitis on systemic inflammation assessed through randomized controlled clinical trials reporting CRP levels 6 months or more following periodontal therapy.
Data Sources and Extraction
The study selection included 26 randomized controlled clinical trials reporting changes amongst 2,579 participants about CRP levels at six months or more after treatment. Six electronic databases were searched up to February 2022. Meta-analyses were performed using random and fixed-effect models.
Data Synthesis
Treatment of periodontitis reduced CRP levels by 0.69 mg/L (95% CI: -0.97 to -0.40) after six months, but limited evidence was retrieved from studies with longer follow-ups. Similar findings were observed in participants with other co-morbidities in addition to periodontitis. Most significant reductions were observed in participants with concentrations of CRP >3 mg/L at baseline.
Conclusions
Treatment of periodontitis reduced serum CRP levels (up to 6 months follow-up) to a degree equivalent to that observed after traditional lifestyle or drug interventions. This evidence supports a causal association between periodontitis and systemic inflammation.
Clinical Relevance
Systemic inflammation drives several chronic diseases and periodontitis could be an unrecognized trigger.
This evidence supports a causal association between periodontitis and systemic inflammation, which could explain the excess risk of future other non-communicable diseases and their complications. Assessment and effective management of periodontitis could be part of routine medical care in the future.