Background
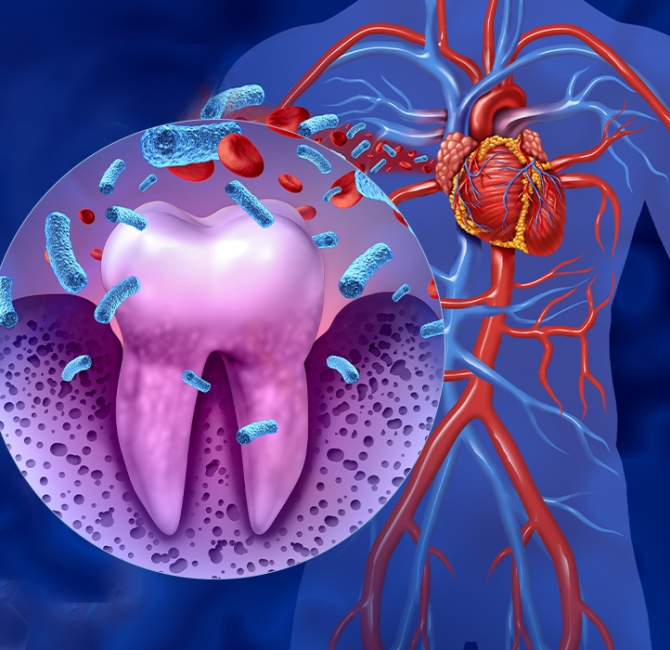
Glycemic control is a key component in diabetes management. Periodontitis is the inflammation and destruction of the underlying supporting tissues of the teeth. Studies have shown evidence of a bidirectional relationship between glycemic control and periodontitis.
Glycemic control can be measured by glycated hemoglobin assay (HbA1c), which shows average blood glucose levels over the preceding three months. It can be reported as a percentage of total hemoglobin or as mmol/mol. Excellent glycemic control in a person with diabetes is approximately 6.5% or 48 mmol/mol.
Treatment for periodontitis involves subgingival instrumentation using hand or ultrasonic instruments. Subgingival instrumentation is sometimes accompanied by local or systemic antimicrobials, and occasionally by surgical intervention for severe periodontitis.
This Cochrane Review is part one of an update of a review published in 2010 and updated in 2015, and evaluates periodontal treatment versus no intervention or usual care.
Objective
The objective of this Cochrane Review was to investigate the effects of periodontal treatment on glycemic control in people with diabetes and periodontitis.
Data collection and analysis
The authors searched six research databases and found 35 relevant trials where people with diabetes and periodontitis were randomly allocated to an experimental group or a control group. The experimental groups received subgingival instrumentation. In some experimental groups, subgingival instrumentation was supplemented with oral hygiene instruction, or other periodontal treatments (e.g., antimicrobials). Control groups received no active treatment or ‘usual care’, which was oral hygiene instruction, support with oral hygiene, and/or removal of plaque above the gingival margin.
The trials randomized 3,249 participants in total. Almost all participants had type 2 diabetes, with a mix of good, fair, and poor glycemic control. Most of the studies were conducted in hospitals. The studies followed up participants for between 3 and 12 months.
Main results
Evidence from 30 trials (results from 2,443 participants) showed periodontitis treatment reduced HbA1c in people with diabetes on average by 0.43% (e.g., from 7.43% to 7%; 4.7 mmol/mol) 3 to 4 months after receiving the treatment compared with no active treatment or usual care. A difference of 0.30% (3.3 mmol/mol) was seen after 6 months (12 studies), and 0.50% (5.4 mmol/mol) at 12 months (one study).
Conclusions
Currently there is moderate-certainty evidence that periodontal treatment using subgingival instrumentation improves glycemic control in people with both periodontitis and diabetes by a clinically significant amount when compared to no treatment or usual care. Further trials evaluating periodontal treatment versus no treatment/usual care are unlikely to change the overall conclusion reached in this review.