Background
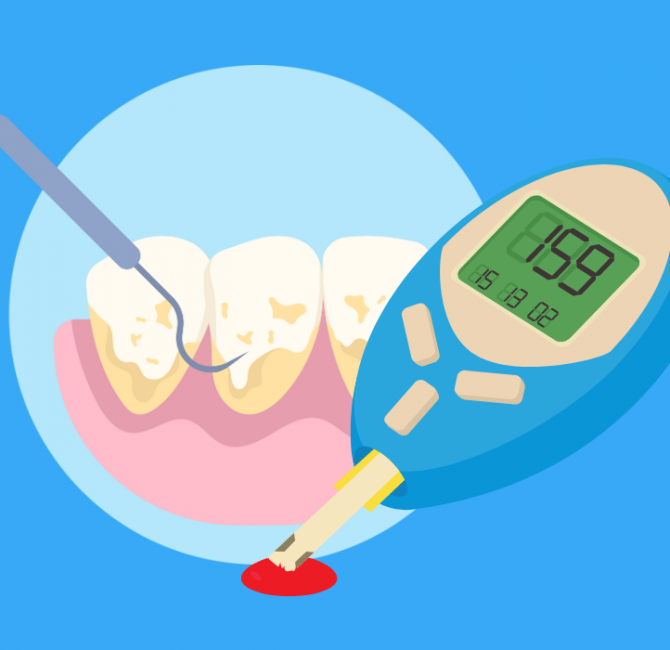
Periodontal disease is one of the most common inflammatory diseases in humans. Periodontitis is a global public health problem impacting oral health, general health, and well-being. Traditionally, periodontitis was considered a local inflammatory disease of the periodontium. Numerous studies have demonstrated associations between periodontitis and various chronic systemic conditions, such as cardiovascular diseases, rheumatoid arthritis, diabetes, Alzheimer’s disease, obesity, and respiratory diseases. However, most of the studies are cross-sectional, making it difficult to establish causality.
Periodontitis and numerous systemic diseases share environmental, lifestyle, and genetic risk factors. Having one noncommunicable disease may increase susceptibility to developing another. The systemic effects of one disease may also serve as risk factors for developing another condition. Both periodontitis and systemic diseases cause a proinflammatory state in the body. Periodontitis is also associated with a prothrombotic state and elevated immunological activity. When viewed as a systemic disease, periodontitis can affect the susceptibility and progression of other systemic diseases and vice versa. Thus, periodontitis is associated with various systemic diseases. A systemic disease is a disorder that affects different organs and systems.
Objective
This paper proposes periodontitis should be considered a systemic disease that impacts an individual’s overall health and well-being.
Inflammatory disease
Periodontitis is a complex, multifactorial inflammatory disease characterized by immune dysregulation and dysbiotic plaque biofilm. Both intrinsic and environmental factors contribute to its development. Intrinsic factors include genetic risk factors, with various genetic variants identified. Environmental factors include lifestyle (e.g., smoking, unhealthy diet, stress), systemic conditions (e.g., diabetes, obesity), and tooth-related factors. Age is also a factor since aging increases susceptibility to any disease due to immunosenescence. Periodontal disease shares many of these risk factors with other chronic diseases.
Proinflammatory and prothrombotic states
Periodontitis is an inflammatory disease of the periodontium. The effects of the inflammation are not localized to the oral cavity, as research indicates C-reactive protein (CRP), a biomarker of systemic inflammation, increases in individuals with periodontitis. Evidence shows nonsurgical periodontal therapy decreases CRP, including a progressive reduction up to 6 months. This evidence supports periodontitis as a systemic disease.
Systemic effects of periodontitis can occur directly through the transmigration of microorganisms, microbial components, inflammatory mediators, such as interleukins (IL-1, IL-6, IL-8) and tumour necrosis factor-alpha (TNF-α), and activated immune cells from the periodontal lesions. Alternately, other organs may respond with inflammatory or aberrant activity to the transmigrated mediators and microbial components. As a result, periodontitis can be considered a systemic disease because of its ability to cause proinflammatory and prothrombotic states and altered immune responses, affecting various body organs.
Systemic diseases
Most noncommunicable diseases share the common characteristic of a proinflammatory state that can exacerbate or influence other chronic diseases. For example, rheumatoid arthritis is a factor for metabolic syndrome and cardiovascular disease (CVD). Inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis, increase the risk of atherosclerotic CVD and diabetes. Chronic obstructive pulmonary disease (COPD) heightens the risk of atherosclerotic CVD. Similarly, periodontitis, as a systemic disease, creates a proinflammatory environment, increasing the risk for other diseases.
Well-being
Health-related quality of life (HRQoL) is a multidimensional concept used to assess how an individual’s health status affects their quality of life. Evidence shows periodontal disease negatively impacts systemic health, and periodontal therapy can improve HRQoL. The effects of periodontal disease on HRQoL are similar to other systemic diseases, as they both can adversely affect physical and mental functioning. Periodontal disease can interact with other systemic diseases to further worsen HRQoL. Additionally, the more severe the periodontitis, the greater the negative impact on quality of life.
Conclusion
This paper proposes periodontitis should be considered a systemic disease. The systemic effects of periodontitis are comparable to those seen in conditions such as rheumatoid arthritis, inflammatory bowel disease, and chronic obstructive pulmonary disease. The proinflammatory state, prothrombotic state, and increased systemic inflammatory indexes in periodontitis are similar to other systemic diseases. These proinflammatory and prothrombotic states are also risk factors for other health conditions. Additionally, individuals with periodontitis experience reduced health-related quality of life.
The findings highlight periodontal disease is not an isolated condition; it has significant systemic effects, impacting overall health and well-being. Collaboration among oral health and medical professionals is crucial to ensure individuals with periodontal disease receive comprehensive care that addresses their oral and systemic health. This collaboration will ultimately improve client outcomes and promote overall health.