Key Messages:
- Periodontitis is a risk factor for cardiovascular disease, and aging plays a mediating role in this association.
- Progression of periodontitis is significantly associated with biological aging, suggesting periodontitis may accelerate the systemic aging process.
- Periodontitis management may delay aging and reduce cardiovascular disease risk.
Introduction
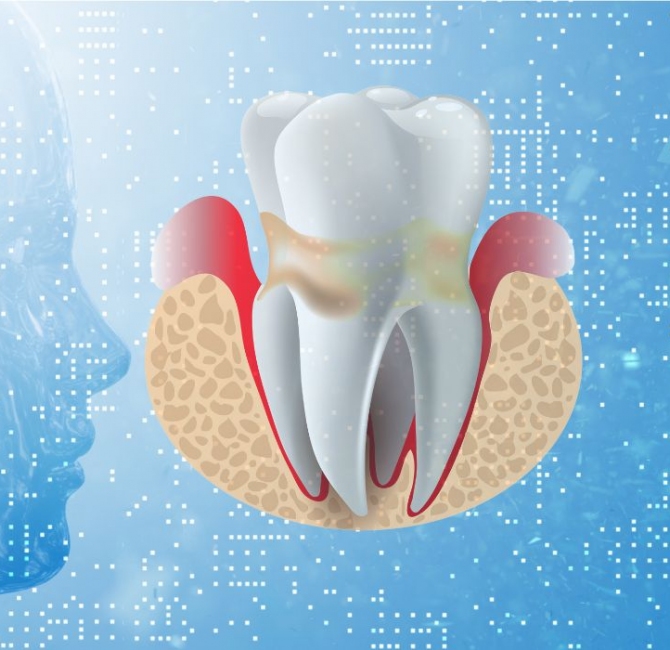
Periodontitis is a chronic inflammatory disease affecting a significant proportion of the global population. The systemic inflammation caused by periodontitis can affect various organs, including the cardiovascular system. Cardiovascular disease (CVD) is a leading cause of morbidity and mortality worldwide. Although the relationship between periodontitis and CVD has been extensively studied, the role of biological aging in this relationship is poorly understood.
Periodontitis and CVD are recognized as diseases of biological aging. Physiological changes from biological aging may affect host-bacterial interactions, exacerbating the incidence and severity of periodontitis. Similarly, biological aging is an independent risk factor for CVD, as biological age-related changes increase susceptibility to cardiovascular issues. Given the impact of biological aging on both diseases, it can be hypothesized that periodontitis may increase CVD risk by promoting biological aging.
Objectives
This study investigated the effect of periodontitis on CVD incidence and the potential mediating role of biological aging. In addition, the causal association between periodontitis, CVD, and biological aging were examined.
Methods
The study utilized data from the National Health and Nutrition Examination Survey (NHANES) to investigate the association between periodontitis and CVD. The study included 3,269 participants with diagnostic information on periodontitis and CVD events. Mendelian randomization (MR) analyses used genome-wide association study databases to explore potential causal relationships between periodontitis, CVD, and biological aging.
Findings
Periodontitis was associated with a higher risk of CVD. Participants with periodontitis had increased levels of biological aging, and elevated levels of biological aging were associated with increased CVD risk. Mediation analyses showed a partial mediating effect of biological aging between periodontitis and CVD risk. MR analysis showed periodontitis played a causal role in increasing the risk of small vessel stroke, while myocardial infarction increased the risk of periodontitis. Additionally, reverse MR analysis showed phenotypic aging can increase the risk of periodontitis, and there is a two-way causal relationship between CVD and biological aging.
Conclusions
Periodontitis is associated with an increased CVD risk, partially mediated by biological aging, with a complex causal interrelationship. Targeted interventions to improve periodontal health may slow biological aging processes and reduce CVD risk.