Introduction
The global use of dental implants has risen significantly over recent decades. This widespread use has subsequently increased the prevalence of peri-implant complications. Peri-implant diseases are primarily biofilm-mediated inflammatory conditions that compromise peri-implant tissues. The two distinct peri-implant diseases include peri-implant mucositis and peri-implantitis.
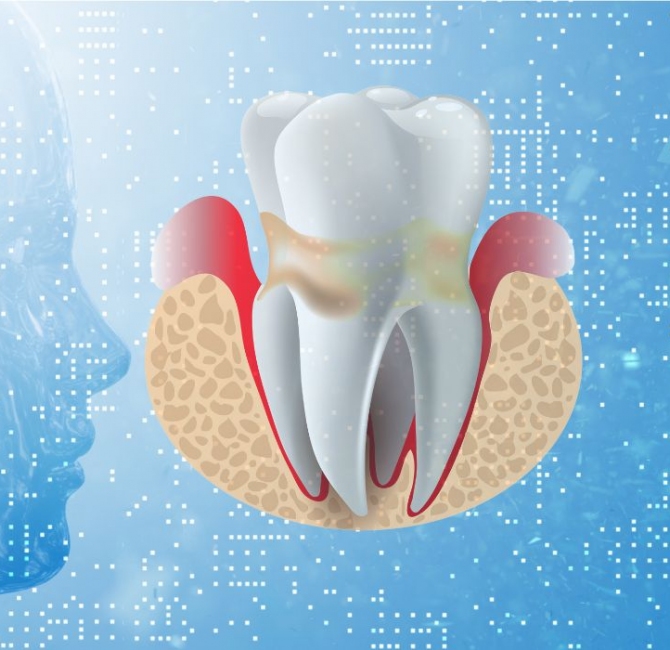
Peri-implant mucositis is characterized by inflammation of the soft tissues around the dental implant, without progressive bone loss beyond the normal physiological bone remodelling. Clinical signs of peri-implant mucositis include bleeding on gentle probing, erythema, swelling, and/or suppuration. If not treated effectively, peri-implant mucositis may progress to peri-implantitis. Peri-implantitis, characterized by persistent inflammation of the peri-implant mucosa and progressive loss of supporting bone, can compromise the longevity of dental implants.
Investigations have been conducted to identify the systemic, behavioural, and site-specific risk factors that contribute to the causes and development of peri-implant diseases and conditions. Efforts have also been made to establish standardized treatment protocols for managing these clinical issues. However, a universally accepted gold standard treatment protocol for the effective and predictable management of peri-implant diseases has yet to be developed.
Objectives
The Academy of Osseointegration (AO) and the American Academy of Periodontology (AAP) consensus summary report synthesized the best available evidence and expert opinion into a framework to prevent and manage peri-implant diseases and conditions.
Methods
Focused questions, addressed in eight systematic reviews, were grouped into two main topics. Group one evaluated systemic and local risk factors and indicators for the onset and progression of peri-implant diseases and their associated defects. Group two focused on therapeutic strategies to manage peri-implant disease, encompassing nonsurgical debridement, implant surface decontamination methods, and surgical interventions. Structured consensus discussions were held to inform evidence-based recommendations.
Results
Various systemic, behavioural, and local factors play a critical role in the onset and progression of peri-implant diseases. Key systemic and behavioural risk factors include a history of periodontitis, smoking, uncontrolled diabetes, inadequate biofilm control, excessive alcohol consumption, obesity, and lack of preventive maintenance appointments. Additionally, implant malposition, unfavourable prosthetic factors, and suboptimal peri-implant soft tissue phenotypical features are relevant site-related factors for peri-implant diseases and peri-implant soft tissue dehiscence.
Nonsurgical debridement and control of risk factors remain the primary approach to treat peri-implant mucositis. This is also the first step to treat peri-implantitis. More advanced cases of peri-implantitis require individualized surgical therapies, such as flap-for-access, resective, reconstructive, or soft tissue augmentation procedures. Supportive peri-implant therapy is essential for long-term peri-implant tissue stability and health.
Conclusions
The findings of this consensus summary report emphasize the importance of comprehensive pretreatment assessments and implementing client-specific preventive strategies to optimize implant therapy success and reduce the risk of peri-implant diseases and related complications.
Detailed flow diagrams were created to guide clinicians through treatment pathways to manage peri-implant diseases and conditions, emphasizing early risk factor identification, tailored treatment protocols, and continued supportive peri-implant therapy to optimize long-term implant therapy outcomes.