Some drugs work well for one person but are ineffective for another; some also produce adverse events for certain individuals but not others. A study, using human gut bacteria and a mouse model, investigates whether our gut bacteria might help explain why.
For many years, scientists have known that the bacteria in our guts play a vital role in digestion.
As technology has advanced, it has become quicker and easier to characterize our microbiome and take a deeper look at its role in health and disease.
However, as more information comes to light, the complex relationship between humans and our resident microbes is becoming ever more convoluted.
Scientists are now investigating gut bacteria’s role in a diverse range of diseases, from Parkinson’s disease to anxiety to heart disease.
Once an obscure niche of medical research, gut bacteria are now firmly in the spotlight.
Now, a further study has examined the potential role our gut bacteria might play in drug metabolism. After all, when we take drugs orally, many are destined to end up in our gut.
Drugs and our gut microbes
Because the microbiome differs from individual to individual, it begs the question of how these variations might impact the way we metabolize these drugs and how they enter the body.
It is well known that drugs do not affect everyone in the same way. In some individuals, a drug might work well; for others, it might require longer to take effect or not work at all; in some people, a particular drug might produce dangerous side effects.
There are many reasons why people respond differently to the same drug, including age, sex, genetics, and diet. So, could the bacteria in our gut also be playing a role?
According to the latest team of researchers to look into this question, our microbiome contains 150 times more genes than our own genome. These microscopic tenants produce a wide array of enzymes, some of which can alter drugs, either activating them or rendering them ineffective.
The researchers set out to uncover more detail about the microbiome’s influence on drugs. Led by Andrew Goodman from Yale University School of Medicine in New Haven, CT, they recently published their findings in the journal Nature.
The group explains that earlier studies have shown how microbes can influence the way that specific drugs work. For instance, sulfasalazine, a drug used to treat ulcerative colitis, relies on gut bacteria to activate it.
Conversely, Eggerthella lenta, a bacterium found in the colon, can inactivate the cardiac drug, digoxin.
However, although scientists have described the microbiome’s impact on specific drugs, Goodman and his colleagues explain that “the molecular mechanisms remain largely unknown.”
Furthermore, the scientific community has yet to describe the exact size and scope of this issue.
Investigating their gene products and more
In the latest study, the authors scrutinized interactions between microbes and drugs by assessing how human gut bacteria metabolize a range of medications. They also set out to identify microbial gene products — primarily enzymes — that might metabolize medicines.
In total, they assessed the abilities of 76 common strains of gut bacteria to alter 271 drugs. The drugs were selected to span a wide variety of types, mechanisms of action, and chemical properties.
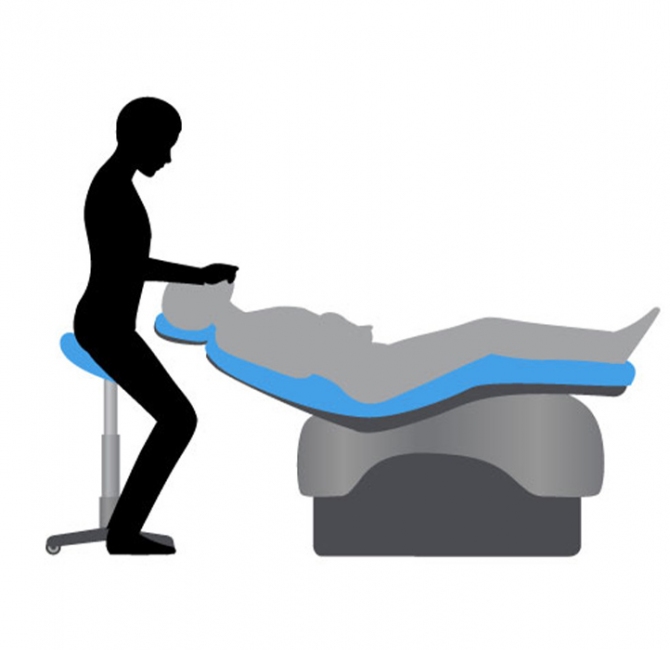
To investigate the interaction further, the scientists used gnotobiotic mice — animals free from microbes.
They found that 176 out of the 271 drugs (64.9%) could be metabolized by gut bacteria, reducing the drug’s concentration significantly. They also showed that each strain of bacteria could metabolize 11–95 types of drug.
They found that by using metagenomic data — the sum of the genes from a given population of bacteria — they could explain the potential of the group or individual bacterial species to alter drugs.
The scientists hope that, going forward, this understanding might help doctors to predict how individuals are likely to respond to drugs. The authors write:“This could provide a means to mechanistically connect microbiome information to interpersonal variation in drug metabolism and toxicity.”
In the future, it might be possible to modify a person’s microbiome to ensure a drug works effectively and reduce the risk of serious adverse events. However, scientists will need to carry out much more research to build up a clearer picture of how these interactions work.
For now, our understanding of the influence of gut bacteria and drug metabolism is still in its infancy. Nevertheless, the findings from this latest study make it seem likely that our gut bacteria are having at least some influence on the medicines we take.